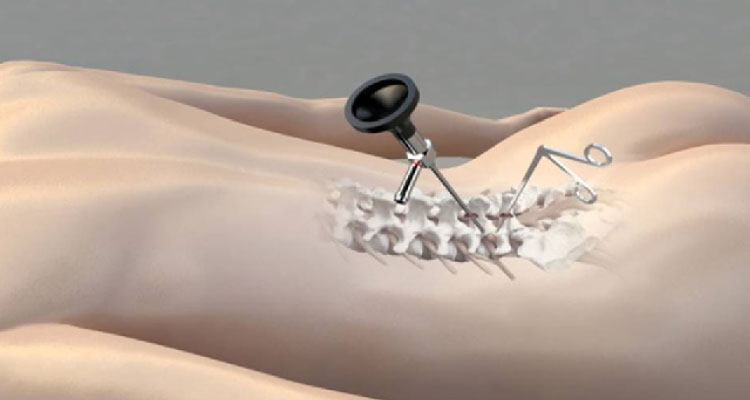
Endoscopic spine surgery is a minimally invasive surgery carried out through an endoscope. An endoscope is a 7 mm tube with a light source and a high-resolution camera lens.
As part of the operation, the surgeon creates an 8mm incision and then carefully splits muscle fibers to allow the endoscope to enter through a small opening in the spine. Using an endoscopic camera, the surgeon can see images of the inside of the body and any pathology that might be present on a monitor. Remove the bone spurs, thicker ligaments, or herniated disc material by inserting small instruments into the working channel. Afterward, the surgeon removes the equipment and sews the wound shut.
Is Endoscopic Spine Surgery Right for You?
You've tried everything to relieve your back pain, but nothing has worked. Endoscopic spine surgery may be the best option for this patient.
A herniated disc, facet joint syndrome, foraminal stenosis, and unsuccessful back surgery can all be successfully treated with endoscopic spine surgery.
What Is the Procedure for Endoscopic Spinal Surgery?
Patients are anesthetized and comfortably placed on the operating table. The surgeon then numbs the surgical site to guarantee the patient's comfort during the procedure.
The physician uses X-ray guidance to route a spinal needle and guidewire to the disc causing the patient discomfort. A 1/4-inch-wide micro-incision is produced. It is done by carefully inserting a pencil-sized cannula through the guidewire and into the spinal disc to create the surgical port. The dilator and guidewire are removed.
Ablation and decompression of damaged spinal nerves are performed using specialized micro-instruments implanted through an endoscope. Surgeons frequently resect herniated discs and bone spurs that could be putting pressure on spinal nerves.
For many, laser spine surgery is a marketing ploy. A side-firing laser and radiofrequency radiation are two of the many surgical tools available to our physicians at DISC.
After surgery, the spinal nerves are decompressed and impinged, freed from pressure and damage. Steroidal injections can be delivered through the scope to improve patient comfort and decrease post-operative inflammatory discomfort. The scope and cannula are withdrawn, and a little stitch is used to put a small bandage on the skin.
Before being allowed to return home, patients are transferred to the recovery area and closely watched for a short period.
What endoscopic spine surgery can do for you
Surgery using endoscopic methods causes minor injury to the surrounding spinal systems than traditional surgery. The surgeon creates a narrow passage for the endoscope by making a skin incision and gently dividing the muscles rather than cutting or tearing them. This method reduces muscular damage and, as a result, the weakening that can result from open spine surgery's typical practice of pulling back muscles.
Because endoscopic surgery is less invasive, general anesthesia is not always required, which reduces some medical risks and improves access to surgery for high-risk patients. Additionally, there is minimal blood loss and a low risk of infection, and the procedures are typically conducted as outpatient surgeries on the same day. Together with the minimally invasive procedure, these advantages result in reduced post-operative pain, a faster recovery, and less need for post-operative narcotic pain medication. Most of the time, after endoscopic spine surgery, our endoscopic patients don't need narcotic pain medications.
How is Endoscopic Spine Surgery different from Minimally Invasive Spine Surgery?
The industry standard is endoscopic surgery is the least invasive method of minimally invasive spine surgery (MIS). As with the MIS microdiscectomy operation, endoscopic spine surgery is just as effective in relieving pain in the spine as endoscopic procedures.
Unlike MIS, endoscopic spine surgery causes minor damage to the patient's muscles and soft tissues, allowing quicker recovery. Endoscopic surgery avoids the lower back's key supporting muscles, so it is popular.
ESS uses a 14-inch incision, smaller than the MIS incision of more than an inch. Smaller surgical incisions and avoiding major back muscles can substantially impact patient outcomes.
Faster than open surgery, endoscopic surgery gives the physician better visibility and access to the spinal nerves and discs because of its low-impact nature. Additionally, ESS does not necessitate general anesthesia, which reduces the risk of complications and expedites the patient's departure from the hospital within 2-3 hours following the operation.
Using endoscopy to do spine surgery is undoubtedly the future of the procedure. As a result, endoscopic fellowships are sprouting up throughout the country. Endoscopic fellowships are becoming increasingly popular among surgeons looking to expand their skillset. Endoscopic spine surgery can effectively, safely, and efficiently treat multiple spinal disorders. More than 93% of the early scientific investigations indicate the efficacy of this treatment.


